When you’re experiencing knee joint pain or discomfort, understanding what’s happening inside can feel like a mystery. Imaging scans are crucial tools for your orthopaedic surgeon to accurately diagnose your condition, from a simple sprain to complex arthritis. Knowing which scan is appropriate and why can help you feel more informed and prepared for your diagnostic journey. This article will demystify the common imaging techniques used for the knee and explain when your specialist might recommend each one.
Understanding the role of imaging
Imaging of the knee joint serves as our eyes inside your body, allowing us to visualise bones, cartilage, ligaments, tendons, and other soft tissues without the need for invasive procedures. It helps confirm a suspected diagnosis, determine the extent of an injury or condition, and plan the most effective course of treatment, whether it’s non-operative management, physiotherapy, or knee surgery.
X-rays: The first look
X-rays are often the first line of defence when assessing knee pain. They use a small amount of radiation to produce images of your bones.
-
- What they show: X-rays are excellent for identifying bone abnormalities such as fractures (e.g., of the patella or tibial plateau), bone spurs, and the narrowing of joint space, which is indicative of arthritis (including osteoarthritis). They can also reveal signs of bone infections or tumours.
-
- When they are used: Your orthopaedic surgeon will typically request X-rays if you’ve had a recent injury like a fall or direct impact, or if you’re experiencing chronic pain that could be related to changes in the bone structure, like progressive knee arthritis. They provide a foundational view before considering more detailed scans.
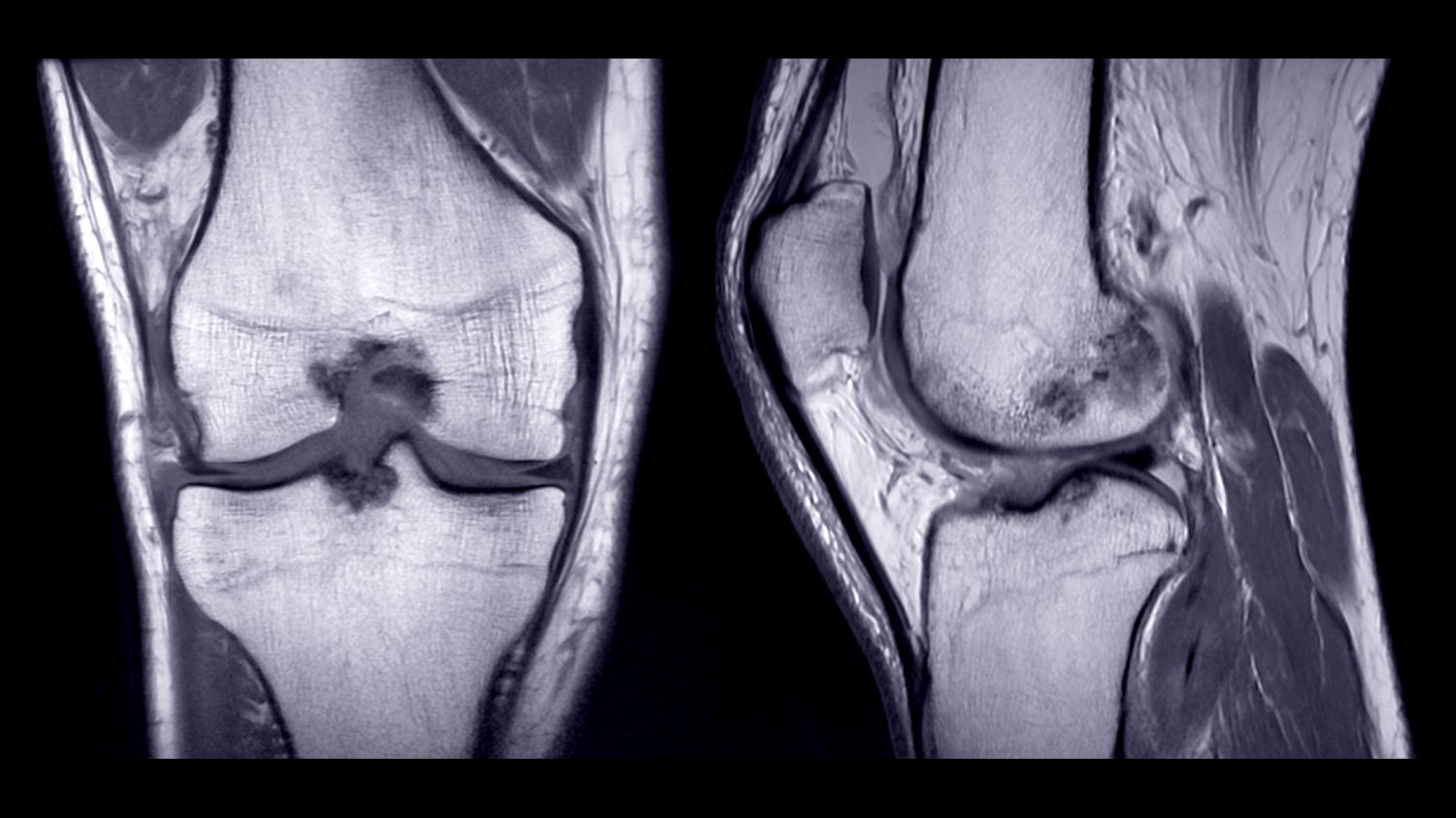
MRI (Magnetic Resonance Imaging): The soft tissue specialist
MRI scans offer a highly detailed view of the soft tissues within and around your knee joint. Unlike X-rays, MRIs do not use radiation; instead, they use a powerful magnetic field and radio waves to create detailed cross-sectional images.
-
- What they show: MRI is invaluable for detecting injuries to ligaments (like an ACL injury or PCL injury), meniscal tears (meniscus tears in the knee), cartilage damage (osteochondral or chondral defects), tendonitis. It can also identify subtle bone bruises or stress fractures not visible on X-rays.
-
- When they are used: An MRI is usually recommended when your orthopaedic surgeon suspects a soft tissue injury that isn’t evident on X-rays, or when a more precise understanding of cartilage or ligament integrity is needed to plan for procedures such as ACL reconstruction, meniscus repair, or complex knee surgery.
CT Scans (Computed Tomography): Detailed bone views
CT scans use a series of X-ray images taken from different angles to create detailed cross-sectional images, offering more comprehensive bone detail than standard X-rays.
-
- What they show: CT scans provide excellent clarity for complex bone fractures, particularly those involving the joint surface (e.g., complex tibial plateau fractures). They are also used for assessing bone alignment, planning complex reconstructive surgeries, and evaluating bone defects. In some cases, a CT scan might be part of the pre-operative planning for procedures like MAKO robotic knee replacement to create a highly accurate 3D model of your unique knee joint for precise surgical planning.
-
- When they are used: Your specialist may order a CT scan if there’s a complex fracture, or when detailed bone mapping is required for surgical planning, especially if considering a total knee replacement or other intricate knee surgery.
Ultrasound: Dynamic real-time assessment
Ultrasound uses sound waves to create real-time images of soft tissues. It’s often used for superficial structures and dynamic assessment.
-
- What they show: Ultrasound can visualise tendons (e.g., quadriceps or patellar tendinopathy), ligaments, fluid collections (bursitis, cysts), and muscle injuries. Its real-time nature allows the orthopaedic surgeon to assess movement and changes in structures under stress.
-
- When they are used: An ultrasound might be used to confirm the presence of fluid, guide injections into a specific area, or assess superficial tendon injuries. It’s less commonly used for deep joint structures compared to MRI.
If you are experiencing knee pain and are unsure about the next steps, we encourage you to Request a Consultation with Dr Richmond for a comprehensive assessment.