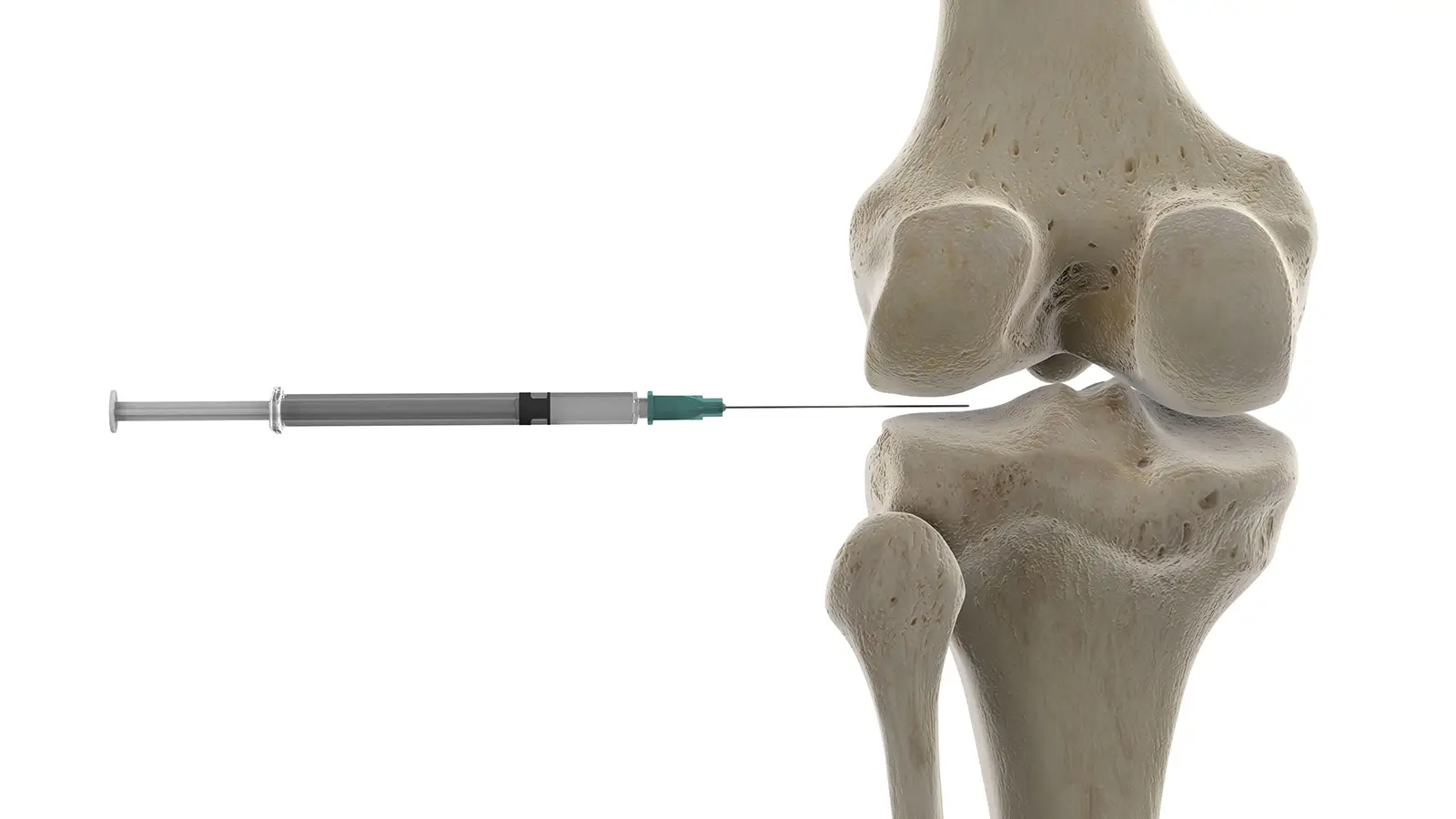
When managing inflammatory joint pain, such as that from arthritis (including osteoarthritis), tendon tears, tendinopathy (inflamed tendons), or bursal/synovial inflammation; steroid joint injections are a common and often highly-effective non-operative treatment option. These injections deliver powerful anti-inflammatory medication directly into the affected joint or surrounding soft tissues. While they can provide significant relief, like any medical intervention, they come with both benefits and risks. Dr Richmond will discuss whether this is a suitable part of your personalised treatment plan.
What are steroid joint injections?
Steroid joint injections, contain a corticosteroid medication combined with a local anaesthetic, are administered directly into a painful joint or around an inflamed tendon. Dr Richmond administers some steroid joint injections in his rooms at the time of consultation(s), other joints are best injected under image guidance i.e., Ultrasound or CT scan, by a Radiologist.
- Mechanism of Action: The corticosteroid works by reducing inflammation, which in turn alleviates pain and swelling in the affected area. The local anaesthetic provides immediate, though temporary, pain relief.
- Common Uses: They are frequently used to treat conditions such as knee arthritis, shoulder arthritis, rotator cuff impingement (bursitis), inflammatory arthritis, and some forms of tendinopathy. For example, an injection may be used for a painful flare-up of knee arthritis that is not yet severe enough for knee replacement surgery, or for a partial rotator cuff tear that is causing irritation and swelling.
The pros: Immediate relief and increased function
For many patients, steroid joint injections can offer significant and rapid benefits.
- Rapid Pain Relief: One of the most compelling advantages is the quick reduction in pain and inflammation, often felt within hours to a few days after the injection. This can provide a much-needed window of comfort.
- Improved Function and Mobility: With pain alleviated, you may experience improved range of motion and an increased ability to perform daily activities, exercise, or engage more effectively in physical therapy. This can be particularly beneficial if pain has been limiting your rehabilitation efforts.
- Targeted Treatment: The medication is delivered directly to the source of inflammation, maximising its effect where it’s needed most and minimising systemic side effects often associated with oral medications.
- Diagnostic Aid: In some cases, a positive response to an injection can help confirm that the targeted joint or structure is indeed the source of your pain.
- Delaying Surgery: For patients not yet ready for orthopaedic surgery (such as a total knee replacement or shoulder replacement), injections can provide symptomatic relief, potentially delaying the need for surgical intervention for months, sometimes years, and occasionally indefinitely.
The cons: Potential risks and temporary nature
While beneficial, it’s important to be aware of the potential drawbacks and limitations of steroid joint injections.
- Temporary Relief: The pain relief from steroid injections is usually temporary, lasting anywhere from a few weeks to several months. They do not “cure” the underlying condition, especially for progressive diseases like arthritis.
- Potential Side Effects: While generally safe, potential side effects can include:
- Post-injection flare: A temporary increase in pain for 24-48 hours.
- Infection: A rare but serious risk, as any injection carries a small risk of introducing bacteria. For this reason, steroid injections are also avoided within 3 months of joint replacement surgery.
- Allergic reaction: Also rare, but possible.
- Skin changes: Localised skin thinning or discolouration at the injection site, uncommon.
- Tendon weakening: Repeated injections into or near tendons can potentially weaken the tendon, increasing the risk of rupture (e.g., rotator cuff tendons).
- Blood sugar spikes: Patients with diabetes may experience a temporary increase in blood glucose levels.
- Limited Number of Injections: Due to the potential for cartilage damage or tendon weakening with repeated use, your orthopaedic surgeon will usually limit the number of steroid injections you can receive in a single joint over a given period (e.g., typically no more than 3-4 per year).
Masking Symptoms: While pain relief is desirable, it’s crucial not to overdo activity during this period, as the pain relief might mask symptoms of ongoing damage or overuse.
If you are experiencing joint pain and exploring your non-operative options, Request a Consultation with Dr Richmond to discuss if a steroid joint injections could be part of your treatment plan.